Using a highly concentrated solution of antibodies against COVID-19 may not be effective in treating the virus, new trial results have found.
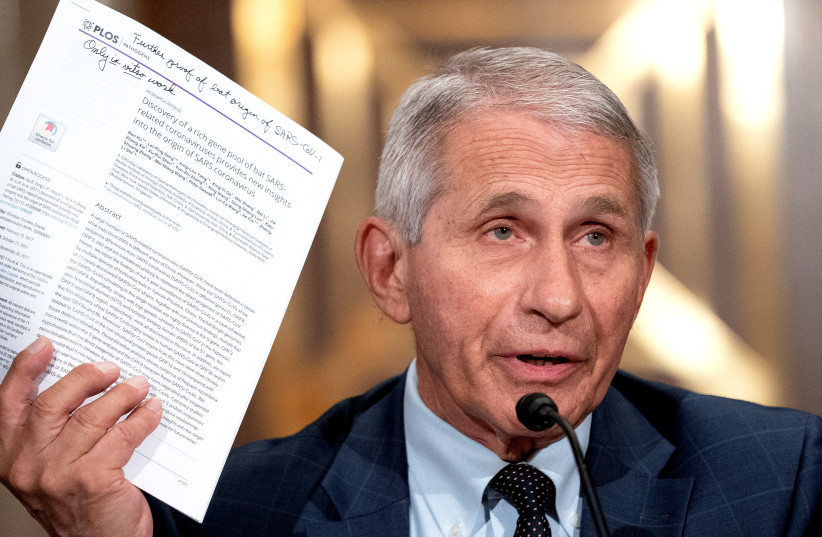
A Phase 3 clinical trial sponsored and funded by the National Institutes of Health's (NIH) National Institute of Allergy and Infectious Diseases (NIAID), which is run by the top US disease expert Dr. Anthony Fauci, studied treating hospitalized COVID-19 patients with a combination of anti-coronavirus hyperimmune intravenous immunoglobulin, or hIVIG, and the drug remdesivir, an antiviral treatment approved by the US Food and Drug Administration (FDA) that is recommended treatment for COVID-19 in certain patients.
The trial was given the name Inpatient Treatment with Anti-Coronavirus Immunoglobulin (ITAC).
However, according to the results of the trial, which were published in the peer-reviewed academic journal The Lancet, using hIVIG with remdesivir has little to no benefit when compared to just using remdesivir alone.
<br>What is hyperimmune intravenous immunoglobulin?

The hIVIG is derived from healthy people who had recovered from COVID-19 and have kept an immune response from the infection. Specifically, this is made into a drug product that is taken from the blood plasma of multiple recovered COVID-19 patients.
Using plasma for antibodies like this is something that, for a large portion of time during the pandemic, seemed to be a promising way of fighting the virus in patients who are already infected.
The hypothesis for using plasma is that the antibodies it contains could neutralize the novel coronavirus, stopping it from replicating and halting tissue damage.
While a small single-center trial had found promising results, this was not successfully replicated.
This study hoped to change that and find an effective treatment regiment.
“In our quest to find safe and effective treatments for COVID-19, we had hoped that adding anti-coronavirus hIVIG to a remdesivir regimen would give the immune system a boost to help suppress the virus early in the course of hospitalization,” Fauci said in a statement.
“Unfortunately, the ITAC trial demonstrated that this strategy did not improve the health of adults hospitalized with COVID-19 and may be harmful for a certain subset of patients. Studies testing this strategy in non-hospitalized adults earlier in the course of infection are underway.”
Further, the study also noted that whether a person naturally generates COVID-19 antibodies before treatment may be a a factor in the safety of this treatment.
<br>Are antibodies ineffective?
Antibodies from blood plasma were once considered a promising treatment against COVID-19. However, studies have shown that this seems to not be the case.
Several studies testing convalescent blood plasma have shown no apparent benefit for treating COVID-19 patients who are severely ill. A US-based trial was halted in March after it was found that plasma was unlikely to help mild-to-moderate COVID-19 patients.
In December 2021, the World Health Organization officially advised against using blood plasma of patients who recovered from COVID-19 to treat sick patients, as it neither improves survival or reduces the need for ventilators based on current evidence.
Another factor is the Omicron variant of coronavirus, which has a large number of uniquely specific mutations that allow it to evade preexisting antibodies.
Shira Silkoff and Reuters contributed to this report.
