People with AIDS might soon have the option to be treated with just a single vaccine dose, according to a new study from Tel Aviv University that shows the potential impact of a new and unique AIDS/HIV treatment.
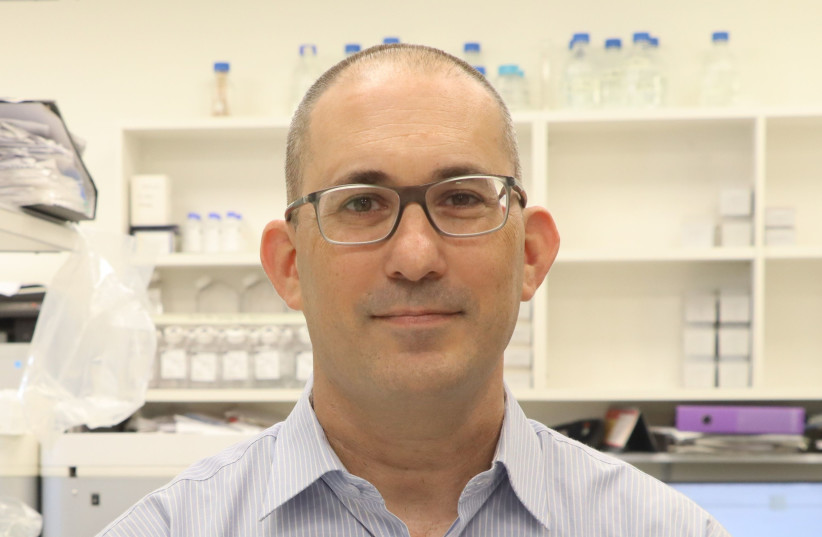
The peer-reviewed study was led by Dr. Adi Barzel and PhD student Alessio Nehmad, both from the TAU School of Neurobiology, Biochemistry and Biophysics, in collaboration with additional researchers from Israel and the United States. It appeared in Nature Biotechnology on June 9.
What is HIV/AIDS
HIV/AIDS (human immunodeficiency virus/acquired immunodeficiency syndrome) was discovered in 1981 and was first reported on in a gay newspaper, The New York Native, on May 1 of that year. HIV was transferred from non-human primates (primarily chimpanzees) to humans in west-central Africa in the early-to-mid 20th century in a process known as zoonosis.
The virus is spread primarily by unprotected sex, contaminated blood transfusions, hypodermic needles or from mother to child during pregnancy.
More than 36 million deaths have been attributed worldwide to AIDS since it was first identified. As of 2020, about 37 million people were living with the disease, primarily in eastern and southern Africa.
While the disease is no longer always fatal, and while many HIV-positive people live full and long lives, currently available treatments do not provide a permanent cure. The research team led by Dr. Barzel aims to change that.
The goal of the research team was to genetically engineer type B white blood cells inside the body of a person with AIDS. Once modified, the blood cells would be able to secrete neutralizing antibodies against the HIV virus responsible for AIDS, eradicating it from the patient’s body.
Type B white blood cells are responsible for generating antibodies against a variety of things including bacteria and viruses. B cells are initially formed in bone marrow but move into the blood and lymphatic system as they mature. From there, they can spread to the rest of the body.
Before modifying the B cells outside the body with which to create a one-time injection, the research team had to first ensure that the B cells were able to generate the desired antibodies. That meant genetically engineering them inside the body.
“Until now, only a few scientists, and we among them, had been able to engineer B cells outside of the body, and in this study, we were the first to do this in the body and to make these cells generate desired antibodies.”
Dr. Adi Barzel
“Until now, only a few scientists, and we among them, had been able to engineer B cells outside of the body, and in this study, we were the first to do this in the body and to make these cells generate desired antibodies,” Barzel said, explaining the process of the study.
The genetic engineering process was done with viral carriers taken from viruses that were modified to not cause harm, but to only carry the necessary gene coded for the antibody into the B cells inserted into the patient.
“All model animals who had been administered the treatment responded and had high quantities of the desired antibody in their blood,” said Barzel. The team, he added, “produced the antibody from the blood and made sure it was actually effective in neutralizing the HIV virus in the lab dish.”
How were the B cells modified?
In order to genetically modify the B cells to produce the antibody, CRISPR gene-editing technology was used. The technology is based on a bacterial immune system against viruses, with the bacteria using the CRISPR systems as a molecular search engine, locating viral sequences and disabling them.
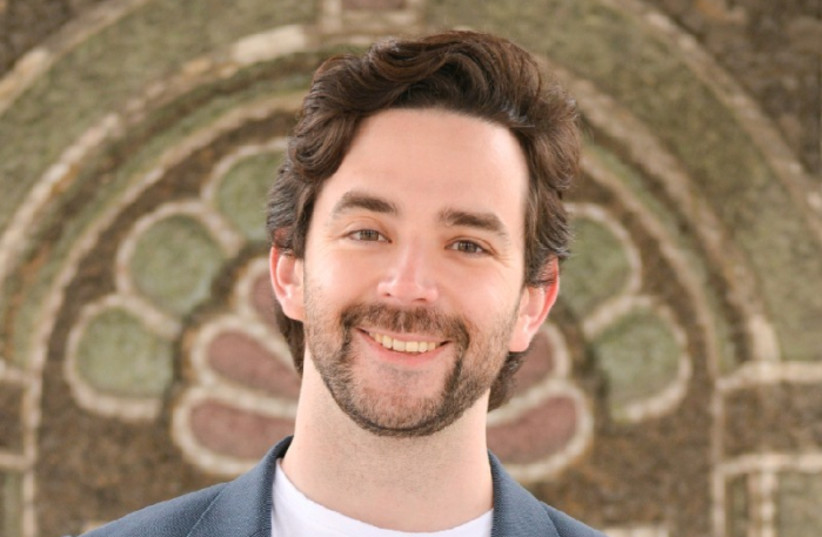
Doctoral student Nehmad explained, “We incorporated the capability of a CRISPR to direct the introduction of genes into desired sites along with the capabilities of viral carriers to bring desired genes to desired cells. Thus, we were able to engineer the B cells inside the patient’s body.”
“We incorporated the capability of a CRISPR to direct the introduction of genes into desired sites along with the capabilities of viral carriers to bring desired genes to desired cells. Thus, we were able to engineer the B cells inside the patient's body.”
Alessio Nehmad
Once the engineered B cells encounter the HIV virus inside the body, the virus stimulates the B cells and encourages them to divide, further spreading the antibodies. Furthermore, if the virus changes or evolves, the B cells will automatically change to combat it, making it the first-ever medication that can actually evolve inside the patient’s body, meaning the virus should not be able to overpower it.
Barzel said, “We are utilizing the very cause of the disease to combat it. Based on this study we can expect that over the coming years we will be able to produce in this way a medication for AIDS, for additional infectious diseases and for certain types of cancer caused by a virus, such as cervical cancer, head and neck cancer and more.”
