Candidiasis is a widespread fungal infection caused by a yeast (a type of fungus) called Candida, and the most common type is Candida albicans. It normally lives in small amounts on the skin and inside the body – in the mouth, throat, gut and vagina – without causing any problems.
The yeast is present at low levels in the bodies of most healthy people, forming part of the microbiome – a diverse spectrum of microbes that reside peacefully in the gut and on the skin. The bacteria living on and inside the body combined with the efforts of the immune system help keep Candida populations under control.
Dangerous yeast rash rises in severity
However, this distant cousin of baker’s yeast is notorious for causing various types of thrush that can be a major nuisance. An overgrowth of the fungus can be painful, itchy, annoying and even – in extreme cases – be deadly. In these severe cases, it can spread to the bloodstream and from there to the kidneys. Such life-threating infections may occur when a person’s immune system has been weakened, for example, by AIDS or by immunosuppressive drugs such as cancer chemotherapy or steroids.
Among patients being treated in intensive care units, it can lead to an invasive infection that may, on occasion, be responsible for a mortality rate of 30% to 50% when systemic candidiasis develops.
Who is most likely to get candidiasis?
Candidiasis common accompanies pregnancy, chemotherapy, diabetes and HIV/AIDS and may appear in the obese, people suffering from dry mouth and stress, in smokers and women taking birth-control pills. Antibiotics, which wipe out many of the beneficial bacteria within our microbiome, can also unleash local or invasive Candida eruptions by providing it with an unfair advantage over other microorganisms. That’s why, for instance, women sometimes develop a vaginal yeast infection after taking antibiotics.
In a study just published today in the prestigious journal Nature Immunology, a research team at the Weizmann Institute of Science in Rehovot headed by Prof. Jakub Abramson uncovered a previously unknown defense mechanism employed by the immune system in fighting Candida infections.
How the body fights back
Until now, the immune cells that got most of the credit for defending the body against Candida were the small, round lymphocytes – a type of white blood cells – of the T-cell type (TH17). These cells were also the ones to take the blame when this defense failed.

In the new study, postdoctoral fellow Dr. Jan Dobeš, working together with colleagues in Abramson’s lab in Weizmann’s immunology and regenerative biology department, discovered that a powerful commando unit of TH17 cells capable of fighting Candida cannot be generated without crucial early support from an entirely different contingent – a subset of rare lymphoid cells known as type-3 innate lymphoid cells (ILC3) that express a gene called the autoimmune regulator (Aire).
The two groups of cells belong to the two different parts of the immune system that – like foot patrols and specialized units – join forces against a common enemy. The Aire-ILC3s – part of the more ancient, innate arm – spring into action almost immediately upon encountering a threat – in this case, a Candida infection. The TH17s belong to the immune system’s more recent, adaptive arm that takes several days or even weeks to respond but launches a much more targeted and potent attack than the innate one.
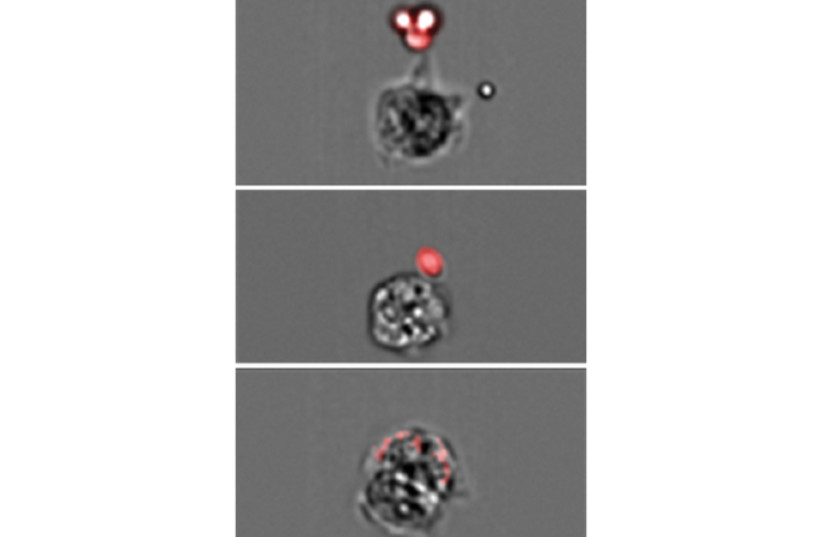
THE SCIENTISTS found that as soon as Candida starts infecting tissues, the Aire-ILC3s surround the yeast, chop them up and display some of the pieces on their surfaces. That’s how these bits are presented to the TH17s, a few of which are generally on call in the lymph nodes, ready for an infection alert. This instructs the specialized T cells to start dividing rapidly, soaring in number from a few lone commandos to several hundred or even thousands of Candida-specific fighters, capable of destroying the yeast at the sites of infection.
“We have identified a previously unrecognized immune system weapon that is indispensable for orchestrating an effective response against the fungal infection,” Abramson declared. “We found an entirely new role for Aire, one that it plays in the lymph nodes – turning on a mechanism that increases the numbers of Candida-fighting T cells,” Dobeš added.
Abramson became intrigued by the fungus because it commonly leads to severe, chronic infections in people with a rare autoimmune syndrome caused by defects in the Aire gene. Abramson’s lab had conducted extensive studies of this gene, helping to clarify its role in preventing autoimmune disorders. That research, as well as studies by other scientists, had shown that Aire-expressing cells in the thymus instruct developing T cells to refrain from attacking the body’s own tissues.
When Aire is defective, T cells fail to receive proper instructions, consequently causing widespread autoimmunity that wreaks havoc on multiple body organs. But researchers didn’t understand why patients deficient in Aire who suffer from a devastating autoimmune syndrome also develop chronic Candida infections.
While trying to complete the Aire puzzle, Dobeš and colleagues found that outside the thymus, Aire is also expressed in a small subset of ILC3s in the lymph nodes. The researchers then genetically engineered two groups of mice – one lacked Aire in the thymus – a small gland in the upper front part of the chest where T cells mature – and the other group lacked it in the ILC3s in the lymph nodes. The first group developed autoimmunity but was able to successfully fight off Candida. In contrast, those in the second group, the ones lacking Aire in ILC3s, did not suffer from autoimmunity but were unable to generate numerous Candida-specific TH17s. As a result, they failed to effectively eliminate Candida infections, so without Aire-expressing ILC3s, the specialized T cells needed for fighting Candida were not produced in sufficient numbers.
These findings open up new directions of research that in the future could help develop new treatments for severe Candida and possibly for other fungal infections. The newly discovered mechanism might, for example, help produce large numbers of Candida-fighting T cells to be used in cell therapy. And if one day, scientists identify the signals by which Aire-ILC3s boost T cell proliferation, these signals themselves might provide the basis for new therapies.
