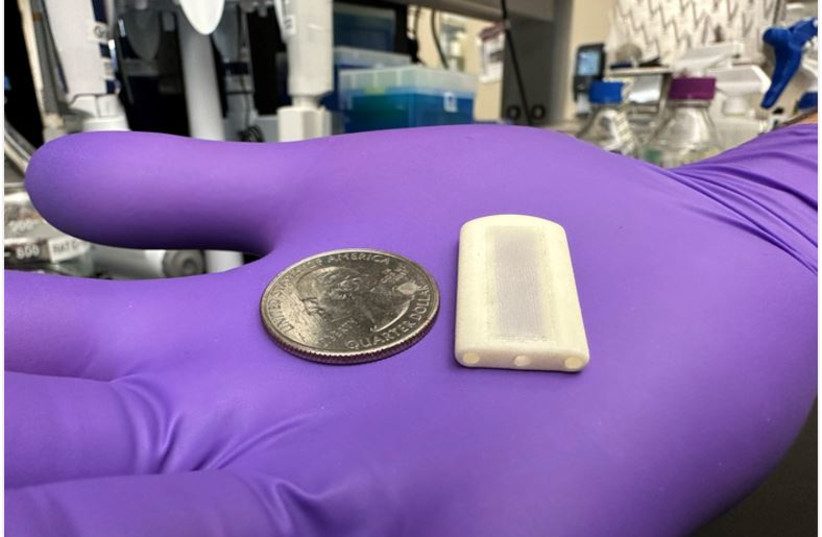
A device the size of an American quarter implanted under the skin could drastically alter the course of treatment for Type-1 diabetes, an incurable chronic condition that impacts many millions of people around the world.
In a study just published in the prestigious journal Nature Communications, a research team led by Houston Methodist Medical Center in Texas delivered islet cells and immunotherapy directly into a 3D-printed device named NICHE, which is similar to a bioengineered pancreas.
Pancreatic islets, also called islets of Langerhans, are groups of cells in the pancreas – an organ that makes hormones to help your body break down and use food. Islets contain several types of cells, including beta cells that make the hormone insulin.
The title of the published study is “Neovascularized implantable cell homing encapsulation platform with tunable local immunosuppressant delivery for allogeneic cell transplantation.”
Cause and treatment of Type-1 diabetes
The treatment restored healthy glucose levels and eliminated Type-1 diabetes symptoms in animal models for more than 150 days while avoiding the severe harmful effects of anti-rejection therapy by administering immunosuppressive drugs only where the transplanted islet cells were located.
Type-1 diabetes is caused by an autoimmune reaction that destroys the islet cells. It can also cause kidney failure. Daily insulin injections are the most conventional treatment, but attaining tight control of glucose levels remains challenging and cumbersome for patients. In more severe cases, patients may need pancreas and kidney transplants or they may qualify for an islet-cell transplant in which the islet cells of a deceased pancreas donor are harvested, processed and then transplanted into the Type-1 diabetes patient’s liver.
These transplants can help improve a patient’s symptoms, but as with all organ transplants, one of the biggest challenges is the need for immunosuppressive drugs for the rest of their lives to avoid rejection of the organ or tissue. Lifelong immunosuppression can lead to patients being vulnerable to infectious diseases and increases the risk of certain types of cancer.
What is the NICHE?
The NICHE, created in the department of nanomedicine at Houston Methodist and tested on lab animals, is a flat device placed under the skin consisting of a cell reservoir for the islets and a surrounding drug reservoir for localized immunosuppression therapy.
It is the first platform to combine direct vascularization and local immunosuppression into a single, implantable device for allogeneic (genetically dissimilar and therefore immunologically incompatible) islet transplantation and long-term Type-1 diabetes management. Direct vascularization is fundamental for supplying nutrients and oxygen for maintaining the viability of transplanted islet cells.
“A key result of our research is that local immunosuppression for cell transplantation is effective,” said Dr. Alessandro Grattoni, who was a leader of the research and is chairman of the nanomedicine department.
“This device could change the paradigm of how patients are managed and can have a massive impact on treatment efficacy and improvement of patients’ quality of life,” he said.
The NICHE incorporates ports for the refilling of drugs as needed. The researchers refilled the drug reservoirs every 28 days, which is comparable to other long-acting drugs clinically available for migraine prevention or HIV treatment.
The team is working on scaling up the NICHE technology for clinical deployment, for which drug refilling may only be needed once every six months. The ability to refill it allows for long-term use in patients. Changes in drug formulations or concentration could extend refill intervals to once every year, aligning with routine physician visits. They will expand the research over the next few years, with the goal of testing the NICHE’s safety in humans in about three years.
