A function of oxytocin discovered in a study published today may be the solution to promoting human heart regeneration after a heart attack.
Oxytocin is a neurohormone with many functions. While most commonly known for generating pleasurable feelings and promoting social bonds, oxytocin also functions in the regulation of ejaculation, sperm transport, and testosterone production in males, and in the regulation of lactation and uterine contractions in females.
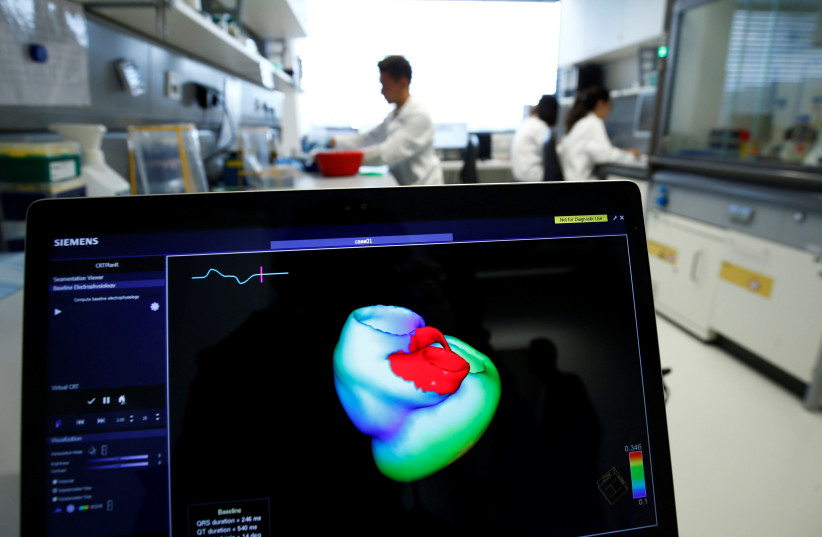
While its functions are many, a study published in the peer-reviewed journal Frontiers in Cell and Developmental Biology by researchers from Michigan State University reveals another purpose that oxytocin possesses in zebrafish and human cell cultures. The findings show that oxytocin stimulates stem cells that are derived from the outer layer of the heart, the epicardium, to migrate into the heart's middle layer, the myocardium, and from there develop into cardiomyocytes which are the muscle cells that generate heart contractions.
“Here we show that oxytocin, a neuropeptide also known as the love hormone, is capable of activating heart repair mechanisms in injured hearts in zebrafish and human cell cultures, opening the door to potential new therapies for heart regeneration in humans,” says an assistant professor at the Department of Biomedical Engineering of Michigan State University and lead study author Dr. Aitor Aguirre.
After a heart attack, an individual's cardiomyocytes normally will decrease greatly. As highly specialized cells, they are unable to replenish themselves.
“Cardiomyocytes are terminally differentiated cells, and as such, their innate regenerative capacity is extremely limited and insufficient to restore function to lost myocardium. Instead, the injured heart typically resorts to wound repair, replacing dead cells with fibrotic scar tissue.”
Dr. Aitor Aguirre, lead study author
“Cardiomyocytes (CMs) are terminally differentiated cells, and as such, their innate regenerative capacity is extremely limited and insufficient to restore function to lost myocardium. Instead, the injured heart typically resorts to wound repair, replacing dead cells with fibrotic scar tissue,” writes Aguirre.
That being said, previous studies have revealed that a subset of cells in the epicardium can regenerate cardiomyocytes along with other heart cells by being programmed to become stem-like cells, called Epicardium-derived Progenitor Cells (EpiPCs). Aguirre explains the EpiPCs as the stonemasons in Europe during the Middle Ages who repaired cathedrals.
However, the production of EpiPCs is sadly ineffective for human heart regeneration under natural conditions.
So, what's missing?
In order to determine how to artificially boost the production of EpiPCs in humans, the researchers looked at the zebrafish. While these fish do not suffer heart attacks, they are known for their extraordinary ability to regenerate organs. Through the proliferation of cardiomyocytes and EpiPCs, they are able to repair their organs, including the heart, even after a predator takes a bite out of it.
The researchers aimed to figure out what it is in the EpiPCs of zebrafish repair that allows them to repair the heart so efficiently.
The team found that the missing piece is oxytocin through examining zebrafish three days after experiencing an injury due to freezing (cryoinjury) to the heart. They observed that the expression of the messenger RNA for oxytocin increases up to 20-fold in the brain. This oxytocin travels to the epicardium and binds to the oxytocin receptor which stimulates cells to expand and develop EpiPCs by triggering a molecular cascade. Then, the newly developed EpiPCs travel to the myocardium of the zebrafish and develop into cardiomyocytes and other heart cells needed to replace the ones that were lost.
What does this conclude about human heart regeneration?
Using a model of human Induced Pluripotent Stem Cells (hIPSCs), the study revealed that oxytocin induces epicardial cell proliferation, which is vital in forming EpiPCs.
“These results show that it is likely that the stimulation by oxytocin of EpiPC production is evolutionary conserved in humans to a significant extent,” says Aguirre. “Oxytocin is widely used in the clinic for other reasons, so repurposing for patients after heart damage is not a long stretch of the imagination. Even if heart regeneration is only partial, the benefits for patients could be enormous.”
“Next, we need to look at oxytocin in humans after cardiac injury,” Aguirre adds. “Oxytocin itself is short-lived in the circulation, so its effects in humans might be hindered by that. Drugs specifically designed with a longer half-life or more potency might be useful in this setting. Overall, pre-clinical trials in animals and clinical trials in humans are necessary to move forward.”
