A protein associated with deadly liver cancer may hold the key to its treatment, according to a new study out of the University of California San Diego.
Activating transcription factor 4 (ATF4) is a protein previously associated with advanced liver cancer, per the peer-reviewed study published in the Journal of Hepatology.
In healthy cells, ATF4 levels are generally low; however, when cells experience stress ATF4 levels rise. Researchers constructed an experiment with mice whose liver cells are deficient in ATF4. The mice were introduced to stressors that promote liver damage and tumor formation.
The researchers found that, surprisingly, mice with lower levels of ATF4 were more susceptible to liver cancer development. This suggests, according to the study, that ATF4 somehow protects against liver cancer.
"ATF4," concluded the researchers, "serves an important protective function in normal hepatocytes (liver cells)."
Further experiments confirmed that ATF4 promoted the proliferation of SLC7A11, a protein that helps maintain liver cell homeostasis. SLC7A11, in turn, suppresses a type of cell death called ferroptosis. By reducing the occurrence of ferroptosis, ATF4 slowed the development of liver cancer in livers that had already experienced a considerable amount of damage.
“Our study suggests that ferroptosis may be the most relevant form of hepatocyte death that leads to inflammation, compensatory proliferation and cancer in the liver,” said senior study author Dr. Michael Karin.
Liver cancer research in Israel
A subtype of immune cells have been found to play a role in the progression of metabolic liver disease, a study from Israel's Weizmann Institute of Science revealed in 2021.
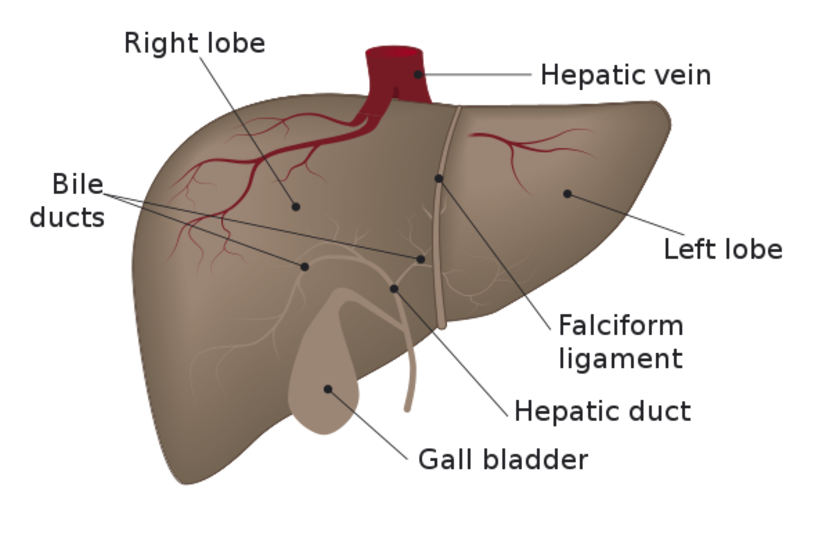
The liver is an essential organ in the body and carries out a wide range of vital functions. However, it is very sensitive to food, and can be thrown into disarray by bad dietary choices and obesity.
An overwhelmingly common condition found among people with obesity is fatty liver, a metabolic condition caused by an excess of fat building up in the liver. This condition itself can be harmless and often have no special symptoms, and can be resolved through simple weight-loss. But for some who don't lose weight or change their lifestyle, it can progress into a far more severe form called non-alcoholic steato-hepatitis (NASH), a condition involving liver-cell death and inflammation that can lead to life-threatening conditions like cirrhosis and liver cancer.
When studying the link between the liver's immune system composition and the pathology of NASH, a team of Weizmann scientists led by Prof. Ido Amit and in collaboration with Mathias Heikenwaelder´s laboratory from the German Cancer Research Center (DKFZ) and the Center for Liver Diseases at Sheba Medical Center discovered the involvement of a certain subtype of immune cells. These cells, known as dendritic cells, are activated in the liver of NASH patients and helps the condition progress further.
The scientists studied the development of this condition in laboratory mice and used new technology developed for single-cell RNA sequencing to study immune changes in the liver. Through this method, they discovered that a specific dendritic cell subtype, called type 1 or cDC1 for short, expands.
They further examined tissue taken from liver biopsies from patients between non-alcoholic fatty liver disease and NASH and saw that the cDC1 count correlated to how great the liver damage was.
These findings, published in the academic journal Nature Medicine, have significant implications for the treatment of fatty liver disease and NASH.
