Many adults suffering from blood cancers who did not develop antibodies from their first dose of the COVID-19 vaccine managed to do so after receiving the booster shot, a new study has found. In addition, receiving antibody alongside the second dose can further shield patients from the virus.
Patients suffering from blood cancers are at high risk of developing a severe case of the disease after being infected with the novel coronavirus SARS-CoV-2, which causes COVID-19. However, the fact that many do not develop immune responses to initial vaccination has raised concerns.
The findings of this study, published in the peer-reviewed academic journal Cancer, raises hopes for protecting these high-risk cancer patients from the global pandemic.
<br>Blood cancers, COVID-19 and vaccine responses
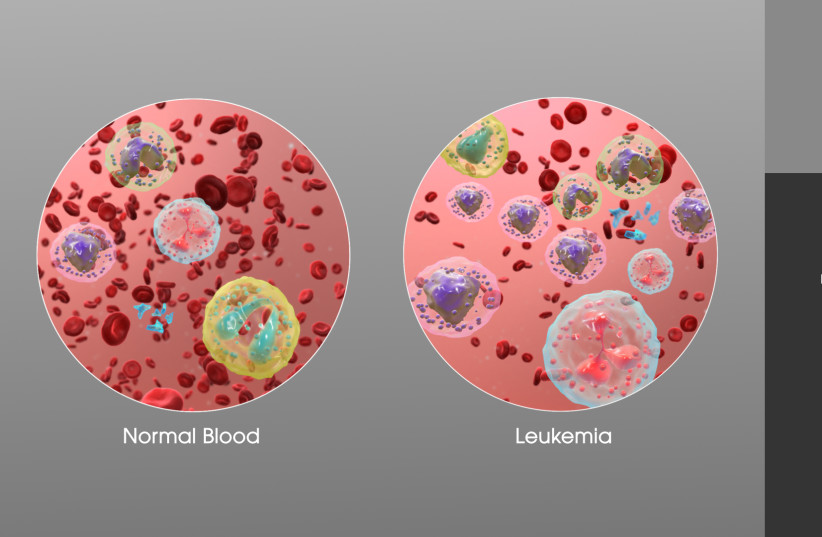
Blood cancers, which the study refers to as hematologic malignancies, are a global problem and come in numerous forms, such as leukemia, multiple myeloma and lymphoma.
According to estimates by the US-based pharmaceutical firm Bristol Myers Squibb in 2020, there are an estimated 1.24 million cases of blood cancers occurring annually around the world, accounting for 6% of all cancer cases. This also results in around 720,000 deaths every year worldwide, making up over 7% of all annual cancer deaths.
According to the National Foundation for Cancer Research (NFCR), the US alone has over 1.3 million people either living with or in remission from a type of blood cancer, with it accounting of 10% of new cancer cases and that on average, one person in the US is diagnosed with blood cancer every three minutes.
The disease is also prevalent in children, with leukemia being the most common type of cancer in children.
As these cancers impact white blood cells and, therefore, the immune system, compounded with the immunosuppressant effects of many cancer treatments, it is unsurprising that blood cancer patients are considered severely immunocompromised and at high risk of contracting severe COVID-19 cases.
When COVID-19 vaccines were first rolled out in places like Israel, and then in countries around the world, priority was given to high-risk individuals, such as the elderly or those who are immunocompromised. This was to ensure that the vaccinated individuals would see high rates of seroconversion, meaning the development of specific antibodies from vaccines.
For many, this is exactly what happened, but patients with blood cancers didn't seem to be so lucky, not developing proper immune responses.
But what about a booster shot? Would that provoke the development of COVID-19 antibodies?
This is what the scientists sought to answer.

The study and results
"This is real world evidence that these actions can save lives."
Dr. Thomas Ollila
To understand the seroconversion rates in blood cancer patients vaccinated against COVID-19, the researchers took a look at serological reports from 378 vaccinated blood cancer patients. Here, they performed a retrospective analysis, tracking their outcomes to see if they ever showed antibodies or ever developed COVID-19.
The study found that for under half (48%) of patients developed antibodies from the first dose of the vaccine. However, that does not mean blood cancer patients were not as at risk of not developing antibodies from the first dose as many feared. Indeed, as the study notes, patients with active cases of blood cancer or who were recently treated, had the lowest seroconversion rates.
But upon receiving a booster shot, antibodies developed in over half (56%) of the patients who didn't develop antibodies the first time.
This was also true for patients currently undergoing active treatment.
There were still cases, though. Overall, 8.8% of patients contracted COVID-19 and 0.8% actually died from it.
But none of those who died were able to develop antibodies, with the study finding that none of those who had antibodies from the vaccine suffered fatalities from the virus.
Despite this, the study was unable to find if the antibodies developed from the second dose actually had higher rates of preventing the patients from contracting COVID-19 in the first place, even if they were shown to have no deaths among them.
But what did have an effect was patients who were treated with tixagevimab/cilgavimab, the preventative COVID-19 antibody cocktail developed by AstraZeneca that is sold under the name Evusheld. This cocktail is used in antibody therapies to target the SARS-CoV-2 spike protein, which stops it from infecting cells.
Indeed, the study found that none of the patients who were given Evusheld ever developed COVID-19.
Now, despite the success of tixagevimab/cilgavimab, which has been approved for use or emergency use in several countries such as the US, UK and in Israel, that doesn't mean it's widely used.
In fact, according to several US media reports from April 2022, 80% of all available doses of tixagevimab/cilgavimab in the US are actually unused on shelves or in warehouses.
But it seems the cocktail is effective, though perhaps not on its own. After all, research is still ongoing regarding tixagevimab/cilgavimab, though research in November 2021 showed that it could provide 83% protection over a six-month period.
But the researchers have hope in it, and recommend combining passive immunization with tixagevimab/cilgavimab with booster shots to shield high risk blood cancer patients from COVID-19 as much as possible.
The results of these findings suggest "the importance of checking antibody levels in these patients and arranging prophylactic [meant to prevent diseases] antibody therapy," explained study leader Dr. Thomas Ollila of Brown University in a statement.
"This is real world evidence that these actions can save lives."
