While many people may take vitamins like Vitamin C and E to improve their health, there may be some dangers in doing so, according to a new study published on August 31.
The peer-reviewed study, published in the Journal of Clinical Investigation, found that the vitamins can stimulate the growth of new blood vessels within cancer cells. These new vessels can aid the cancer in growing and spreading across the body.
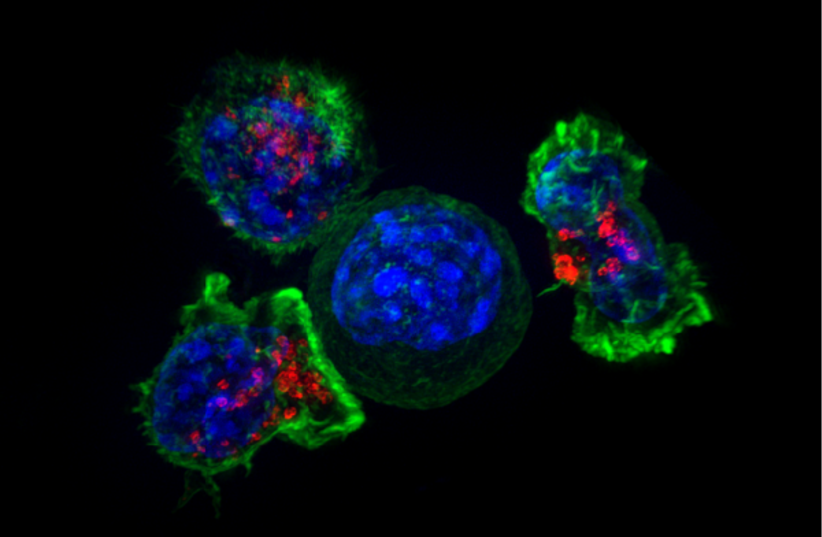
Cancer tumors require oxygen supply and nutrient-rich blood to grow new blood vessels. The process is known as "angiogenesis."
Should people take supplements?
Antioxidants usually work by utilizing unused oxygen from other cells, which reduces the amount of oxidative stress. Oxidative stress can damage DNA and cause increase the risk of cancer.
“We’ve found that antioxidants activate a mechanism that causes cancer tumors to form new blood vessels, which is surprising since it was previously thought that antioxidants have a protective effect,” said author Martin Bergö to New Atlas. “The new blood vessels nourish the tumors and can help them grow and spread.”
“There’s no need to fear antioxidants in normal food, but most people don’t need additional amounts of them,” said Bergö. “In fact, it can be harmful for cancer patients and people with an elevated cancer risk.”
Vitamins E and C in particular can raise the risk of lung cancer because they stabilize the BACH1 protein, which can cause the cancer to spread. This can happen when excessive levels of antioxidants are introduced into a person’s diet, or when mutations occur in tumors, activating the production of antioxidants.
The researchers were able to discover the role of the antioxidants while looking at lung cancer on organoids taken from patients. The same observations took place on breast tissue, kidney tumors, and in experiments on mice.
“Many clinical trials have evaluated the efficacy of angiogenesis inhibitors, but the results have not been as successful as anticipated,” said author Ting Wang
“Our study opens the door to more effective ways of preventing angiogenesis in tumors,” Wang said. “For example, patients whose tumors exhibit high levels of BACH1 might benefit more from anti-angiogenesis therapy than patients with low BACH1 levels.”
“The next step is to examine in detail how levels of oxygen and free radicals can regulate the BACH1 protein, and we will continue to determine the clinical relevance of our results,” continued Wang. “We’ll also be doing similar studies in other cancer forms such as breast, kidney and skin cancer.”
