Researchers have presented scientific evidence that age is simply a number, and a person's true body age can vary from one individual to another, regardless of their birth year. Led by researcher Michael Snyder from the Stanford University School of Medicine, a team has identified four key "age identifiers" – metabolic, immune, hepatic (related to the liver), and nephrotic (related to the kidneys).
These factors determine how certain parts of the body age at a faster rate than a person's biological age and may indicate future health concerns.
"Our research provides a comprehensive understanding of how we age, by examining various molecules and conducting multiple tests over several years on each participant," Snyder explained in a report published in January 2020. "This allows us to identify distinct patterns of aging at the molecular level, with significant differences among individuals."
To gather empirical evidence, the researchers closely monitored 43 healthy men and women aged between 34 and 68 over a two-year study period.
They collected samples of feces, blood, genetic material, bacteria, proteins, and other metabolic byproducts during a minimum of five health assessments, tracking changes in biological molecules over time.
Through extensive testing, the team identified 608 molecules that could be used to predict potential age-related health problems. Subsequently, they classified these biomarkers into four classes of "age identifiers."
"The term 'age identifiers' goes beyond mere labeling," Snyder emphasized. "It helps individuals focus on risk factors for their health and identify areas where they may encounter future problems."

Four age markers
Metabolic: Individuals with an "aging" metabolism are more prone to developing heart disease, obesity, and type 2 diabetes due to the accelerated aging of their metabolic rate – the collection of chemical reactions in the body's cells responsible for converting food into energy. Although at a higher risk for weight-related illnesses, individuals with a higher metabolic rate than their age group may still possess a stronger immune system compared to younger individuals.
Immune: This "age identifier" refers to individuals with an immune system that ages faster than the rest of their body. The faster aging of the immune system often triggers inflammation throughout the body and increases the likelihood of autoimmune diseases such as rheumatoid arthritis, lupus, type 1 diabetes, and multiple sclerosis.
Hepatic: Hepatic concerns individuals whose livers age faster than their chronological age. The liver is a vital organ responsible for detoxifying the blood from harmful substances such as alcohol and drugs. As it ages rapidly, its functions diminish, rendering individuals more susceptible to cirrhosis and non-alcoholic fatty liver disease.
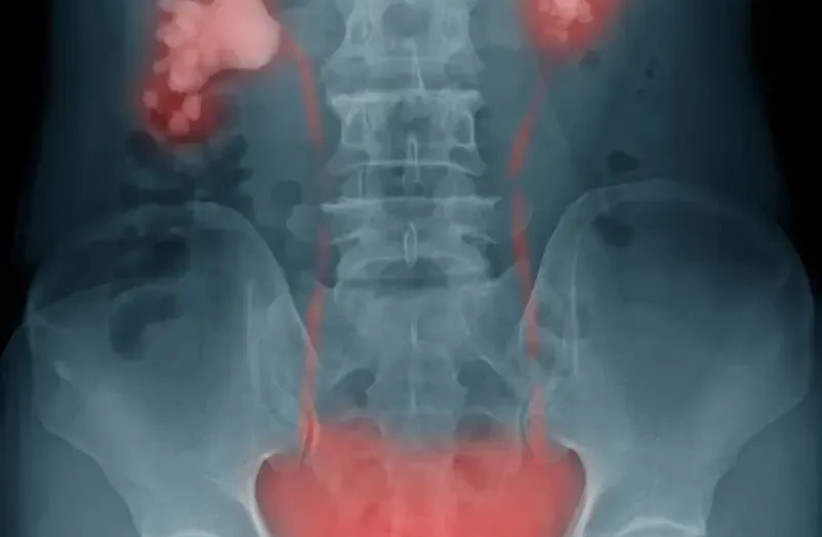
Nephrotic: Nephrotic pertains to kidney health – the organs responsible for filtering waste from the blood and producing urine while maintaining fluid balance and blood pressure regulation. Individuals with kidneys that age at a faster rate may be prone to high blood pressure and kidney failure later in life.
It is important to note that despite the grim reality of poor health in old age, Snyder emphasized that these "age identifiers" do not solely determine one's fate. The fact that a person's metabolism or kidneys may mature faster than their chronological age does not necessarily mean they will have a shorter lifespan. Instead, these "age identifiers" serve as a means for individuals to make lifestyle improvements and lead healthier lives.
Suggestions include weight loss, quitting smoking and alcohol consumption, and monitoring blood pressure and glucose levels to prevent diseases before they manifest.
"Our research shows that it is possible to positively influence the aging process," Snyder assured. "Participants who embraced healthier lifestyles were able to slow down the aging of their bodies."
"Many participants saw reductions in hemoglobin A1c after making changes, including weight loss and dietary modifications," the study reads. "Some participants who experienced decreased creatine levels, indicating improved kidney function, incorporated statins (prescription cholesterol-lowering drugs) into their routines."
